2025/2026 Essential Guide to Veterinary SOAP Notes with Practical Examples

In veterinary practice, accurate documentation is key. Between appointments, emergency cases, and ongoing paperwork, it is impossible to keep patient notes organized. That's where veterinary SOAP notes come in.
They simplify record-keeping using a structured approach that saves time and confusion. In 2025, tools such as Acorn.vet take this even further, with automation, real-time dictation, and templates for modern clinics.
Knowledge of SOAP veterinary formats today means being ahead in tomorrow's veterinary practice. To understand how they help, let’s take a step back and explore what veterinary SOAP notes are and why the entire industry relies on them.
What are Veterinary SOAP Notes?
A veterinary SOAP note is a method of clinical case recording in a structured way. SOAP is an acronym for Subjective, Objective, Assessment, and Plan; a four-part framework applied in both medicine and veterinary fields.
- Subjective (S): Client reporting, behavior, and symptoms.
- Objective (O): Quantifiable information such as vitals, laboratory, and imaging.
- Assessment (A): Your professional opinion and possible diagnoses.
- Plan (P): Recommended treatments, medications, and follow-up measures.
Using the SOAP format is what creates consistency and clarity in each patient record. It enables team members to quickly know what's done, what's planned, and what's next.
Now that the structure is clear, let’s discuss why this four-part note isn’t just paperwork. It’s the foundation of confident patient care.
Why SOAP Notes Matter in Veterinary Practice?
Good veterinary SOAP documentation improves communication and continuity of care. Each note links your team together, making sure everyone is on the same page and no key step is missed.
For rotating or new personnel, SOAP notes vet guarantees that treatments are consistent. They are also crucial in case reviews, insurance claims, and audits. Apart from compliance, brief notes help establish client trust and demonstrate professionalism.
To take documentation to the next level, clinics are now utilizing advanced veterinary scribe software, allowing for faster and smoother note-taking without compromising accuracy.
But, technology alone isn’t helpful if you are not aware of the techniques of writing SOAP notes. Let's find out how to actually write a SOAP note that's complete and efficient.
How to Write Veterinary SOAP Notes (Step-by-Step)
Effective writing of veterinary SOAP notes is all about finding a balance between structure and detail. Every section has a different purpose and should naturally lead into the next.
Here's a step-by-step SOAP template:
- Subjective: Write down what the pet owner describes: symptoms, changes in diet, or behavior.
- Objective: Record measurable information such as temperature, weight, or blood tests.
- Assessment: Describe findings to make a diagnosis or list possible conditions.
- Plan: Record medication, procedures, follow-up, or diagnostics.
Following this SOAP structure guarantees simplicity and standardization. Pre-formatted veterinary SOAP templates can also be used for faster input and reduced error.
Now, before proceeding any further, let us highlight a few errors you should avoid while making these notes.
Common Errors To Avoid in Veterinary SOAP Notes
Veterinary SOAP notes can sometimes contain errors, but they're easy to fix. To make your notes better, avoid these common mistakes when documenting in the Subjective or Assessment categories. Be specific when writing down owner observations (Subjective) and your list of problems (Assessment).
Omitting follow-up arrangements or missing recheck dates can similarly undermine your notes. Delaying documentation until the end of the day often results in lost information and decreased accuracy.
By avoiding these common errors, veterinary SOAP notes can be clearer, precise, and accurate. Now, let's have a glance at some SOAP notes examples that demonstrate it in practice.
Veterinary SOAP Note Examples
Example 1: Canine Wellness Visit (Bella – Labrador Retriever)
|
Section |
Details |
|
S (Subjective) |
Name: Bella Age: 5 years Breed: Labrador Retriever Sex: Female (Spayed) Reason for visit: Annual wellness exam Concerns: Occasional vomiting after meals Appetite: Normal Water consumption: Slightly increased Activity level: Active, playful Diet: Regular commercial diet HW/Flea/Tick prevention: Up to date Current medications/supplements: None reported Reactions to vaccines/medications: None reported |
|
O (Objective) |
Temperature: Normal Heart Rate: Normal Respiratory Rate: Normal Body Condition Score (BCS): Normal Hydration: Adequate Eyes/Ears/Oral Cavity: Normal Cardiovascular: Normal Respiratory: Normal Abdomen: Soft, non-painful Musculoskeletal: Normal Integumentary: Healthy Lymph Nodes: Normal Urogenital: Normal Neurological: Normal |
|
A (Assessment) |
General condition: Healthy Findings: Polydipsia (increased water intake) Immediate concern: Occasional vomiting Differentials: Dietary sensitivity, early GI irritation, or behavioral polydipsia |
|
P (Plan) |
Diagnostics: None indicated at this time Treatment: Not required; maintain hydration Diet: Offer smaller, more frequent meals; consider mild diet adjustment Follow-up: Re-evaluate in 2 weeks or sooner if vomiting or water intake increases |
Example 2: Feline Upper Respiratory Infection (URI)
|
Section |
Details |
|
S (Subjective) |
Name: Luna Age: 3 years Breed: Domestic Shorthair Sex: Female (Spayed) Reason for visit: Sneezing and nasal discharge for 5 days Concerns: Nasal congestion, watery nasal discharge, mild eye redness Appetite: Slightly decreased, still drinking water Water consumption: Normal Activity level: Slightly reduced Diet: Indoor diet, no recent changes Exposure: Indoor-only cat, no new animal contact Vaccination status: FVRCP booster overdue by 2 months Current medications: None reported Reactions to vaccines/medications: None reported |
|
O (Objective) |
Temperature: 103°F (mild fever) Eyes: Watery discharge, mild conjunctival redness Nose: Congested, clear discharge present Lungs: Clear on auscultation Hydration: Adequate Body weight: Stable Heart rate: Normal Respiratory rate: Normal |
|
A (Assessment) |
General condition: Mildly ill but stable Findings: Upper respiratory infection signs Differential diagnoses: Feline herpesvirus-1, Calicivirus, secondary bacterial infection |
|
P (Plan) |
Diagnostics: Not required at this stage Medications: Antiviral (e.g., famciclovir) as needed Supportive care: Encourage hydration and soft food intake Environmental management: Use humidifier or steam therapy for nasal congestion Home care: Clean nasal and eye discharge with warm saline Monitoring: Observe for pus in discharge, loss of appetite, or lethargy Follow-up: Recheck in 5 days or sooner if symptoms worsen |
These soap note samples demonstrate how brief, structured notes keep your employees in sync. But repeatedly having to type them out is tedious, which is where the veterinary AI scribe comes in.
How AI Is Redefining Veterinary SOAP Notes
Breakthroughs in veterinary AI scribe technology have revolutionized the manner in which veterinarians document cases. With voice-to-text software and AI-powered SOAP note AI, you can dictate notes while conducting exams.
These programs capture and format your words in the form of a SOAP note, automatically filling in templates and marking omissions. That means more time for patients, fewer mistakes, and complete documentation each time.
Artificial intelligence-based veterinary scribe software is especially helpful in high-volume clinics, where speed and accuracy both go hand-in-hand.
As these tools continue to evolve, clinics are discovering that not all veterinary AI scribes are the same. Some platforms are designed for modern, fast-paced practices. That’s where Acorn.vet really stands out. Moving on, let's address why Acorn.vet is among the finest in voice-to-text software.
Why Use Acorn.vet for Veterinary SOAP Notes?
Acorn.vet is an all-inclusive digital resource for modern-day veterinarians. It provides intelligent SOAP note AI support, pre-editable veterinary SOAP templates, and seamless integration with the benefits of medical record software systems.
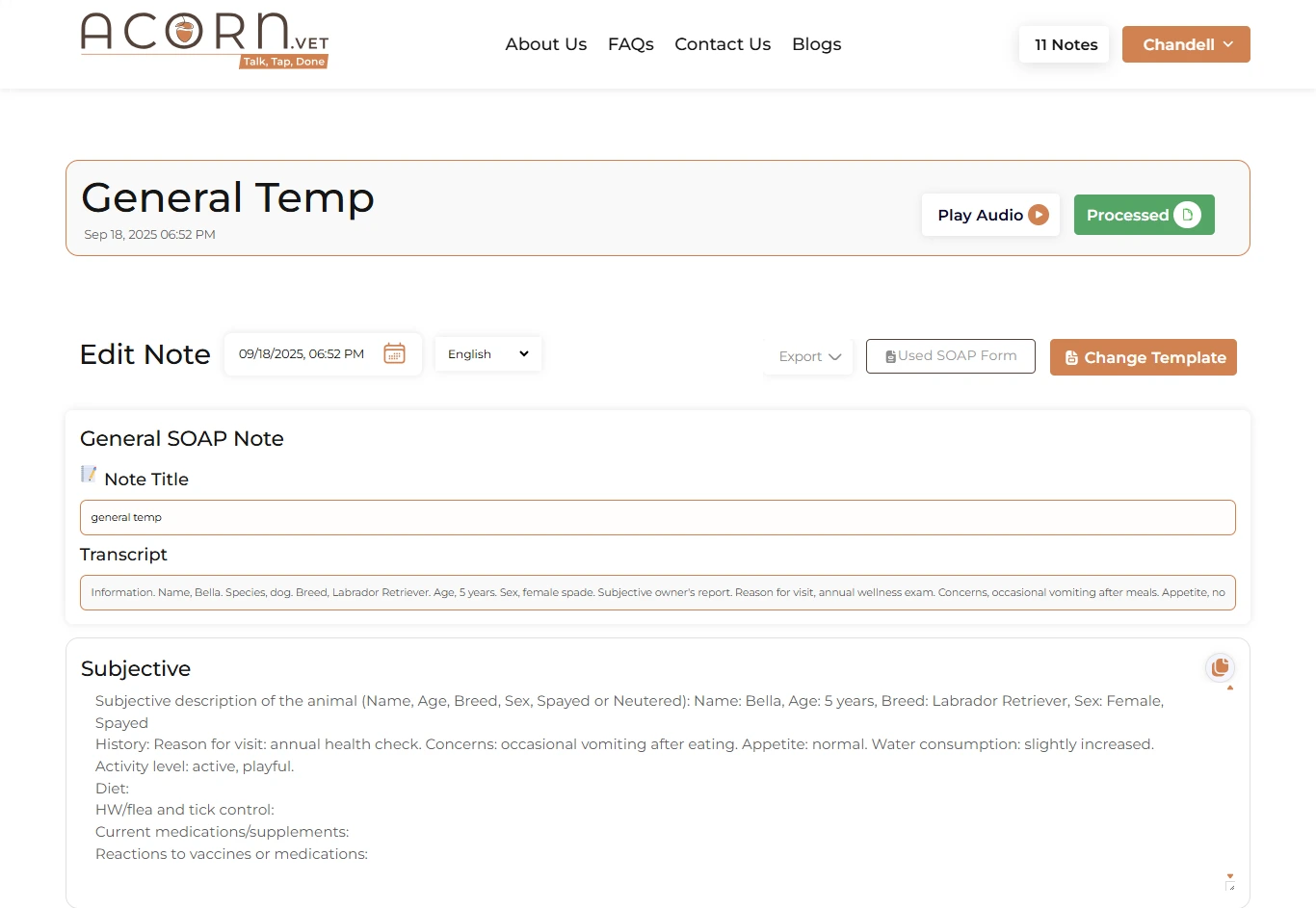
The technology is focused on automation and customization, allowing vets to create consistent, professional notes in minutes. With secure cloud storage and simplified navigation, Acorn.vet facilitates the elimination of stress related to record-keeping.
By integrating innovative veterinary scribe automation and effective veterinary AI scribe technology, Acorn.vet guarantees no detail is ever overlooked.
Conclusion
Precise veterinary SOAP notes enable efficient diagnosis and treatment planning for the best patient care. They improve communication, safeguard your practice, and enhance patient outcomes.
With smart solutions powered by AI, such as Acorn.vet, you're able to work smarter. The future of soap veterinary documentation is smart, fast, and fueled by automation.
FAQs
How to write a veterinary SOAP note?
Start with the Subjective portion on client observations, followed by Objective findings such as exam findings or lab results. Add your Assessment, including diagnosis and rationale, and finish with an in-depth Plan of treatment and follow-up.
Why is SOAP used in veterinary practice?
SOAP ensures brief, consistent recording in every patient case. SOAP helps efficient team communication, tracking of progress, and documentation that reinforces professional practice.
Are there common errors or pitfalls in the writing of SOAP notes?
Yes. Excessive use of jargon, failure to include details within the Assessment, or waiting too long to record can decrease note quality. Keeping a clean template and completing notes in a timely manner makes all the difference.
Can AI or an AI assistant assist in writing SOAP notes for veterinarians?
Yes. Software like Acorn.vet uses veterinary AI scribe tools to reduce time spent on note-taking. They capture verbal dictation, format records in real-time, and reduce labor.
What is SOAP in veterinary medicine?
SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan; the four pillars of quality veterinary SOAP notes that facilitate proper, organized patient documentation.
